Hawaiʻi Overdose Initiative
- About
- Current & Emerging Drug Threats
- How to Protect Yourself and Others
- Data and Statistics of Hawai‘i’s Overdose Situation
- How to Get Involved with HOI
What is the Hawaiʻi Overdose Initiative?
The Hawai‘i Overdose Initiative (HOI) was launched in January 2025 in response to the public health crisis in the community and its reflection in the growing number of substance-related overdoses and deaths in Hawaiʻi.
In recent years, we have seen (1) the continued growth of fentanyl access in the illicit drug supply; (2) the rise of fatal and nonfatal poisonings due to psychostimulant and polysubstance-related deaths, not just from opioids only; and (3) the growing prevalence of co-occurring substance use and mental health disorders and conditions.
The HOI has a mission that includes all facets of today’s drug epidemic, not just opioids, and seeks to adopt a structure to maximize cross-disciplinary collaboration to craft strategies that reflect community needs across the state. Multi-sector collaboration and commitment is essential to an integrated and effective response. Building on lessons learned, the HOI expands on previous partnerships with the community.
Hawaii Overdose Initiative Action Plan
On January 9, 2025 a consortium was held by the Hawai‘i State Department of Health, Alcohol and Drug Abuse Division (ADAD) and included: government agencies, health care professionals, community groups, advocates, and substance use treatment and prevention providers. This was the nucleus for the formation of the Hawaiʻi Overdose Initiative Action Plan (in progress). This plan is meant to evolve and adapt over time to changes that occur in Hawaii’s socioeconomic landscape.
Implementation of the plan involved the formation of Action Teams to discuss and propose recommendations for ADAD’s next steps. The Action Teams (AT) are listed below.
- Equitable Access to Care
- Culturally Responsive Systems
- Collaborative and Sustainable Communities
- Harm Reduction and Public Safety
- Strengthening Workforce and Resources
- Data Infused Decisions
Current & Emerging Drug Threats
Methamphetamine
Methamphetamine – A highly addictive central nervous system stimulant also categorized as a psychostimulant remains the leading contributor to overdose deaths in Hawai‘i, with more than 75% of fatalities stimulant-related. From 2023 to 2024, meth-involved deaths surged by nearly 50% rising from 214 to 275 deaths.
Signs and Symptoms of a Stimulant Overdose
- Dilated pupils
- Dizziness
- Tremor
- Irritability
- Confusion
- Mood swings
- Nausea or vomiting
- Rapid breathing, fast heart rate or arrhythmia
- Overheating or excessive sweating
- Hypertension (high blood pressure)
- Chest pains or tightness
- Panic or extreme anxiety
- Hallucination
- Psychosis
Illegally-made Fentanyl
Overdose deaths involving illegally-made fentanyl alone (no other opioids or stimulants) have declined, dropping from 43 deaths in 2023 to 28 deaths in 2024. This decrease could be attributed to the availability and saturation of Naloxone as well as Fentanyl Test Strips, but this does not mean the fentanyl crisis is over. Instead, fentanyl is increasingly found in combination with stimulants like methamphetamine, creating a dangerous polysubstance environment.
The following are signs and symptoms of an opioid overdose:
- Unconsciousness or inability to awaken.
- Slow or shallow breathing or difficulty breathing such as choking sounds or a gurgling/snoring noise from a person who cannot be awakened.
- Fingernails or lips turning blue/purple. For lighter skinned people, the skin tone may turn bluish purple; for darker skinned people, skin tone may turn pale/grayish or ashen.
Polysubstance Use – (Opioids and Stimulants)
The information listed below comes from the CDC’s Stimulant Guide.
How is a stimulant overdose different from an opioid overdose?
- People experiencing stimulant overdose are often conscious and may be breathing quickly. They may need assistance in reducing overheating and overstimulation. Naloxone is NOT effective in treating a stimulant overdose. However, if there is the potential that opioids have been consumed, either because someone is unconscious and not breathing, and whether drugs were mixed or unknowingly contaminated, naloxone may be lifesaving.
- People experiencing an opioid overdose are difficult to rouse and typically suffer from dangerously slow or no breathing.
How to Protect Yourself and Others
Responding to a Stimulant Overdose
If you suspect someone is experiencing a stimulant overdose, call 911.
- Call 911 if a seizure does not resolve within 5 minutes, if the person experiences multiple seizures in a row, if they have never had a seizure before or if they have difficulty breathing or waking up after the seizure.
- Remain calm and help the person in distress. Talk to them calmly to let them know what the person responding is doing.
- Help the person lie down safely without falling or hitting their head, if possible.
- Remove nearby objects, including eyeglasses, to reduce the risk of injury from sudden, involuntary movements.
- Do not put anything in their mouth or between their teeth.
- Do not try to restrain the person’s movements.
- Naloxone will not work to reverse a stimulant overdose, but it is safe to give someone naloxone if you’re unsure if they took opioids. If in doubt, give naloxone
Responding to an Opioid Overdose.
This information comes from SAMHSA’s Overdose Prevention and Response Toolkit
- IF THE PERSON DOES NOT RESPOND OR YOU ARE NOT SURE WHAT TO DO NEXT, CALL 911.
STEP 1 – ADMINISTER AN OPIOID OVERDOSE REVERSAL MEDICATION (OORM).
- Naloxone is a life-saving medication designed to rapidly reverse an opioid overdose.
- If overdose is suspected and the person is unresponsive, give an OORM as quickly as possible and then call 911.
- Naloxone does not cause harm if given to a person who is not experiencing opioid overdose.
- If the person does not start breathing or otherwise respond after 2-3 minutes, administer a second dose of naloxone. Continue to give doses every 2-3 minutes until the person starts breathing.
STEP 2 – SUPPORT THE PERSON’S BREATHING.
- If you can, provide rescue breaths.
- When a person overdoses, they stop breathing and this can quickly cause damage to the brain and other organs.
- You may use a medical oxygen delivery device, if available.
STEP 3 – WAIT FOR EMERGENCY MEDICAL SERVICES TO ARRIVE
- Naloxone wears off after 30-90 minutes and overdose symptoms may return.
- Encourage the person to receive treatment from EMS and/or go to an emergency department
Overdose Prevention Tips
- Don’t Use Alone. Have someone nearby, a trusted person can call 911 or give naloxone if needed.
- Avoid Mixing Substances. Combining stimulants with opioids or other drugs greatly increases overdose risk. Stick to one substance at a time.
- Start Low, Go Slow. Use a small amount first to test potency. Avoid large doses or rapid use.
- Stay Hydrated and Rested. Drink water, eat regularly, and get sleep. Long periods without food or rest can make stimulant effects more dangerous.
- Test Your Drugs. Use fentanyl test strips to check powders, pills, or crystals before use. If fentanyl is detected, reduce your dose, keep naloxone nearby, and alert someone who can help.
- Know What You’re Using. Illicit drugs are often mixed with other substances or contaminated with fentanyl. Counterfeit pills that look like prescriptions are common.
- Keep Naloxone Accessible. Naloxone can reverse opioid overdoses—even if fentanyl wasn’t expected. Learn how to use it and share with others.
- Seek Support Without Judgment. Local harm reduction programs, primary care providers, and findtreatment.gov can help—whether you want to stop, cut back, or just stay safer.
Data and Statistics of Hawaiʻi’s Overdose Situation
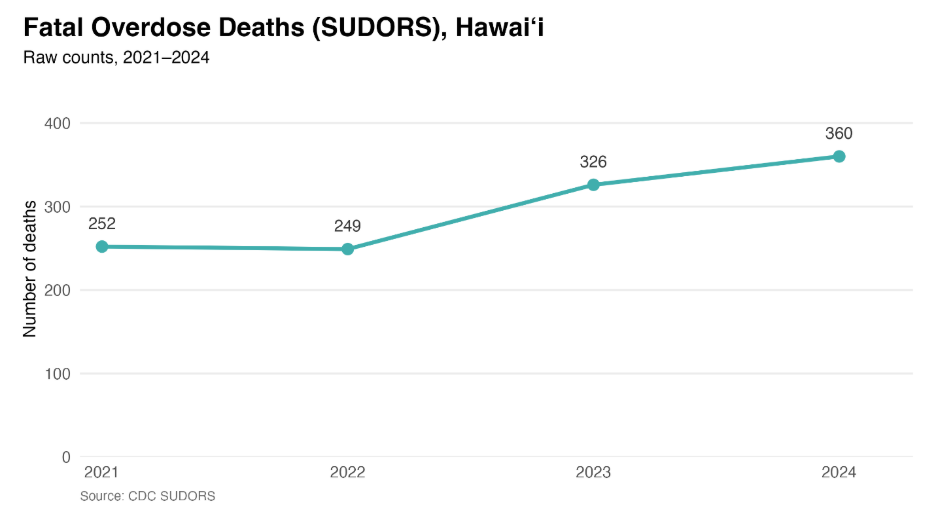
Hawai‘i is facing a growing overdose situation that has worsened in recent years. According to the Centers for Disease Control and Prevention (CDC)’s State Unintentional Drug Overdose Reporting System (SUDORS)*, unintentional drug overdose fatalities in the state rose from 252 deaths in 2021, to 360 deaths in 2024 – an increase of approximately 42.9% (Table 1).
Below are infographics developed by the Motivation for Change (M4C) Substance Use and Prevention Group at the University of Hawai‘i at Mānoa, Department of Public Health Sciences.
Table 1
* In 2016, the State Unintentional Drug Overdose Reporting System (SUDORS) began as part of CDC’s Enhanced State Opioid Overdose Surveillance (ESOOS) program, to provide comprehensive data on opioid overdose deaths. In 2019, SUDORS expanded to collect data on all drug overdose deaths in 47 states and the District of Columbia as part of CDC’s Overdose Data to Action (OD2A) program. In 2023, SUDORS expanded again to include 49 states and the District of Columbia as part of CDC’s OD2A in States program. Each of these 50 funded jurisdictions collects and abstracts data on unintentional and undetermined intent drug overdose deaths from 3 required sources: 1) death certificates (DC); 2) coroner/medical examiner (CME) reports (including scene evidence, witness reports, and autopsy reports); and 3) postmortem toxicology (Tox) reports for entry into a web-based CDC platform that is shared with the National Violent Death Reporting System (NVDRS).
Table 2
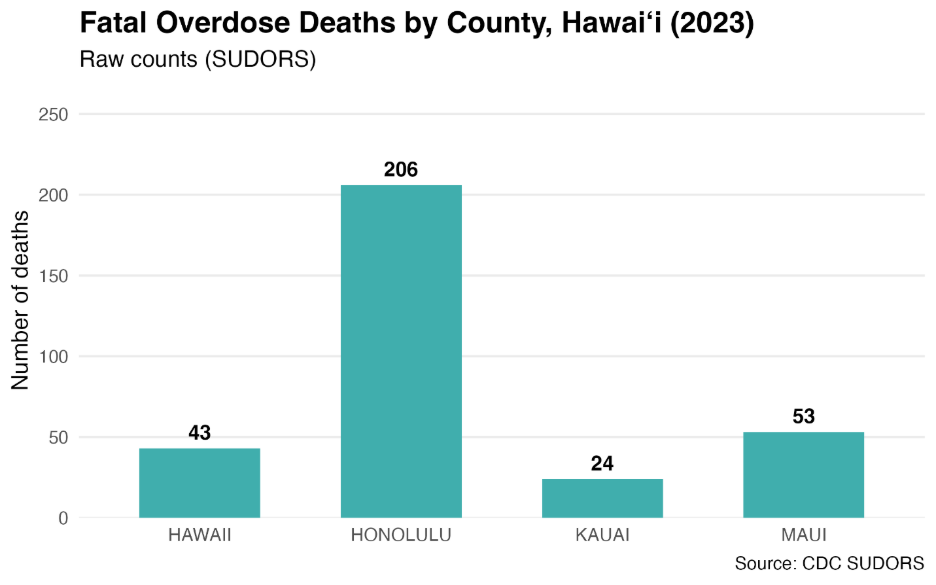
Table 3
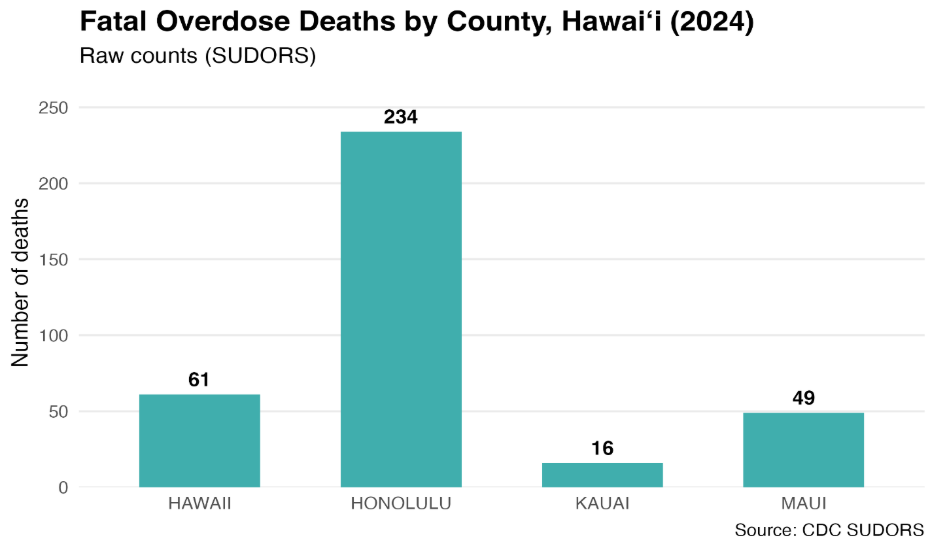
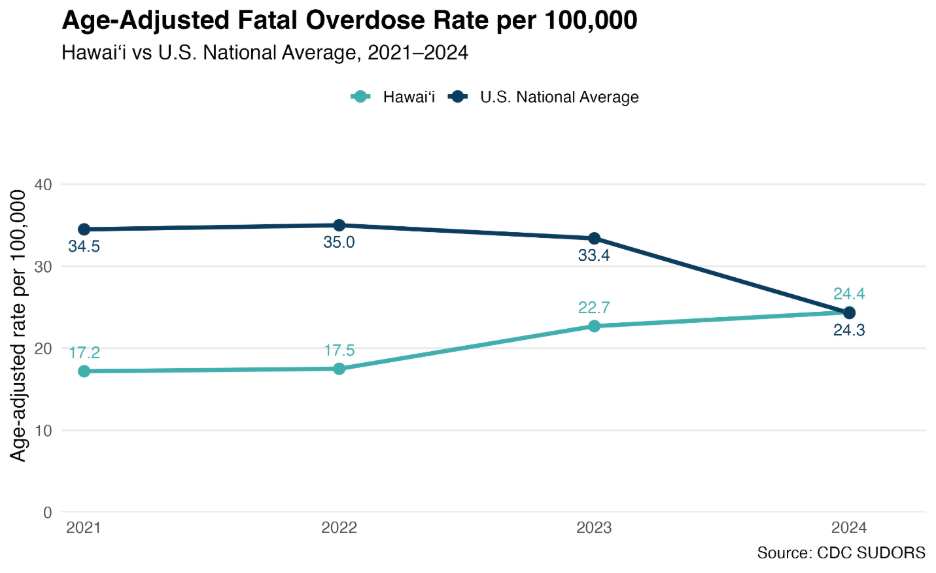
Table 4
In SUDORS, jurisdictions report occurrent drug overdose deaths (i.e., all overdose deaths that occurred within the jurisdiction irrespective of decedent residence). Thus, rates on the SUDORS dashboard are calculated using occurrent deaths for the numerators. From 2020 to 2024, most (~94%) occurrent deaths included in the SUDORS dashboard occurred in the decedent’s jurisdiction of residency, although this percentage varied for a small number of jurisdictions. Even though SUDORS captures occurrent deaths (both resident and non-resident), occurrent population estimates are generally not available; therefore, rates on the SUDORS dashboard are calculated using resident population estimates for the denominators. In general, resident population estimates appear to be a reasonable proxy for the total population (current resident plus temporary/itinerant) in most jurisdictions. Prior comparisons of rates using occurrent deaths and resident deaths in SUDORS yielded similar results; therefore, the use of resident population-based denominators is recommended as the best/most feasible approach for calculating rates with SUDORS data. The burden of occurrent overdose deaths relative to the jurisdiction population size can be helpful for informing local resource allocation and prevention efforts.
Citations:
Centers for Disease Control and Prevention. State Unintentional Drug Overdose Reporting System (SUDORS). Final Data. Atlanta, GA: US Department of Health and Human Services, CDC; [2026, January, 8]. Access at: https://www.cdc.gov/overdose-prevention/data-research/facts-stats/sudors-dashboard-fatal-overdose-data.html
Centers for Disease Control and Prevention. Nonfatal Drug Overdose Surveillance and Epidemiology Syndromic Surveillance (DOSE-SYS) System. Atlanta, GA: US Department of Health and Human Services, CDC; [2026, January, 8]. Access at: https://www.cdc.gov/overdose-prevention/data-research/facts-stats/dose-dashboard-nonfatal-surveillance-data.html
Resources
HAWAI‘I CARES
Hawai‘i CARES 988 is a 24/7, free support service for help with crisis, mental health, and substance use. Call or Text 988 Learn More
FIND TREATMENT
FindTreatment.gov is a free, confidential, and anonymous resource developed by the Substance Abuse and Mental Health Services Administration (SAMHSA) to help individuals find mental health and substance use disorder treatment across the United States and its territories. Learn More
NALOXONE
The Alcohol and Drug Abuse Division provides free naloxone to government agencies, community partners, and non-profits in Hawai‘i who would like to obtain naloxone. Learn more here: https://osp.hawaii.gov/naloxone/
How to Get Involved with HOI
If you are interested in providing input to the Hawai‘i Overdose Initiative or any of the Action Teams, please send an email to [email protected]. The teams will meet regularly May 2025 through June 2026 and their recommendations used to inform the Alcohol and Drug Abuse Division.
Contact:
- For Data related inquires: [email protected]
- For HOI related inquires: [email protected]